
Dental professionals see many patients a day and provide a variety of different procedures requiring them to use specific body movements and positions for long periods of time. This increases the prevalence of musculoskeletal disorders among dentists and if chronic and severe, can in some instances reduce the longevity of a clinician’s dental career. Many dental professionals accept that in the realm of health and wellbeing, prevention is always better than a cure. In this article, concepts of dental ergonomics and stretching will be discussed to allow dental professionals to practise with greater ergonomic safety and prevent work-related musculoskeletal disorders from occurring and ensure longevity in a dental career.
Work-related musculoskeletal disorders (WMSDs) include pain or damage to muscles and surrounding body tissues in the neck, shoulders, back, arms and legs.1 Dental professionals have been found to be at a higher risk of WMSDs compared to other professions given dental practice involves repeated unidirectional twisting of the trunk (repetitive movements), working in static postures for prolonged periods of time without rest (prolonged static postures), awkward work postures, less flexibility and less core strength (muscular imbalances). This can in turn degrade the quality of patient care, decrease work satisfaction and in some cases affect quality of life or end a career early.2
Research shows there are five areas to consider to prevent dental professionals to suffer from WMSDs:
- Dental ergonomics
- Stress management
- Myofascial treatment
- Chairside stretching
- Muscular endurance training
Dental Ergonomics
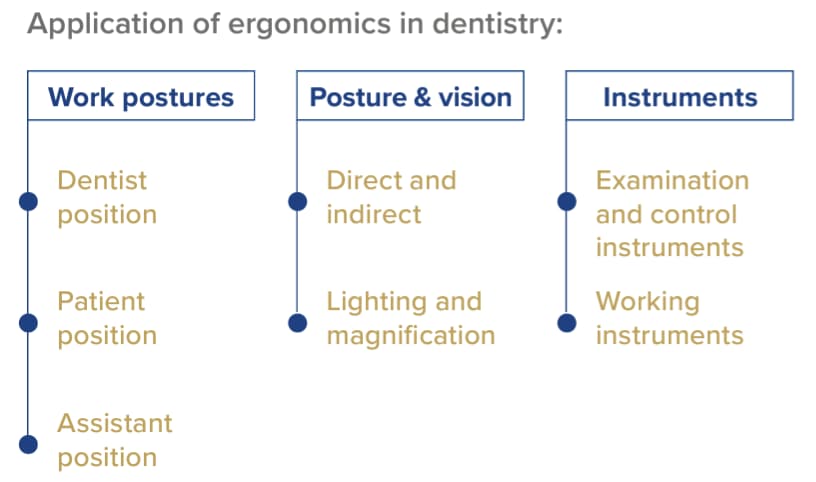
The International Ergonomics Association (IEA) defines ergonomics (or human factors) as “the scientific discipline concerned with the understanding of the interactions among humans and other elements of a system, and the profession that applies theoretical principles, data and methods to design, in order to optimise human well-being and overall system performance”. Ergonomics in dentistry should aim to strike a balance between keeping the dental professional healthy and providing efficient treatment. It also means preventing WMSDs by enabling the dentist to adopt a more natural and comfortable posture, achieving patient-friendly treatment, improving treatment efficiency, and achieving treatment accuracy. Figure 1 from the FDI Ergonomics and Posture Guidelines for Oral Health Professionals below illustrates the main application of ergonomics in dentistry to consider.
One of the most important considerations regarding optimising the work posture of a dental professional is the correct selection of dental stools to sit on and operate each day. Some dentists use a traditional dental stool tilted at a 15° angle however research has found that this can be insufficient to maintain the right lower back curvature in the spine unless there is continual contact with the backrest. Saddle stools are now becoming a more popular ergonomic choice as they open up the hip angle wider than traditional stools so the body is positioned halfway between sitting and standing. However, these tools are not ideal for clinicians who have a pre-existing condition of altered lumbar curve or excessive curvature of the lower back as this can worsen the pain and condition. For these cases, a hybrid saddle stool can be recommended which has a flat seat pan and achieves the steep thigh angulation via a triangle-shaped seat, or cut-out areas, where the thighs can slope steeply downward.4 Having the right stool allows a clinician to maintain an ideal posture in line with ideal positioning of the patient and dental chair.
Another important factor to consider in dental ergonomics is having the correct vision of the patient’s mouth to harmonise posture and vision together. This is achieved through a combination of having appropriate illumination and magnification of the patient’s mouth or dental field of view. To help have a more accurate field of view, dental loupes or dental microscopes can be used. The most ergonomic option to improve the dental field of view is a dental microscope that allows the dentist to maintain the ideal posture throughout the whole procedure, provides excellent illumination and can filter between a range of magnifications depending on the procedure. The main disadvantage of microscopes however is they are quite bulky and not easily portable and are quite costly. The second best option is a magnified set of dental loupes combined with a dental loupe light. There is a plethora of designs and types of dental loupes and dental loupe lights ranging from head gear apparatus to eye glasses as well as flip-up loupe configurations to a fixed through-the-lens (TTL) option. Of all the design options available, the most ergonomic option is the refractive loupe which provides a refracted, angulated view of the dental field whilst allowing the dental professional to maintain ideal posture and minimise prolonged neck bending and chin tilting. A benefit of dental loupe lights compared to the overhead chair light is the fact that the illumination is much brighter, focussed beam and also provides an orange, composite light filter to prevent the setting of composite during restorative procedures without compromising field of view. Although dental loupes are more portable and cheaper than dental microscopes, their main disadvantage is a fixed magnification or field of view. This means a dental professional may require multiple pairs of dental loupes if they require a higher magnification for procedures such as endodontic treatment.
The ergonomic use and design of dental instruments must also be considered so optimal finger, hand and wrist position can be maintained during dental procedures. The use of a dental mirror not only provides retraction of the dental tissues but importantly allows the indirect view of maxillary teeth and mucosal tissues to ensure clinicians do not strain the neck and back by bending in awkward positions to get a direct view of maxillary field of view. Most dental instruments and handpieces are now ergonomically designed with large diameters (10mm) or textured grips for added comfort to be optimally held in a pen-grip position without straining the fingers and thumbs from excessive gripping force.
Stress Management
Aside from the obvious physical and mental strain dental professionals experience from treating patients for prolonged periods of time, management of emotional stress is also important to prevent WMSDs. Chronic stress from conflicts with interpersonal relationships or emotional stress lead to breathing changes and cause the shoulders and back to hunch into a poor posture. This over time can lead to strain and pain in the middle and lower back, possibly affecting the ability for the dental professional to provide optimal care of their patients. Ensuring good stress management through adequate rest breaks between long appointment periods, engaging in other hobbies outside of dentistry and seeking stress management tools from psychological professionals can help reduce the likelihood of unnecessary back strain.4
Myofascial treatment
Myofascial tissue is the connective tissue that provides support to the muscles and bones. With muscle overuse from prolonged strain of muscles during dental practice, combined with dehydration, the fascia in the muscles can get trapped together, leading to formation of hyperirritable knots in the muscle known as trigger points. Trigger points are characteristically sore to touch and can lead to referred pain to other parts of the body. These areas can also feel tight due to the bundling of myofascial tissue together which can be quite painful and in some cases can be exacerbated with exercise. Pain medication often is not able to provide relief and requires physical intervention to release the muscle knots. This can be achieved through appropriate stretching or physical therapy in the form of a massage.5
Chairside Stretching
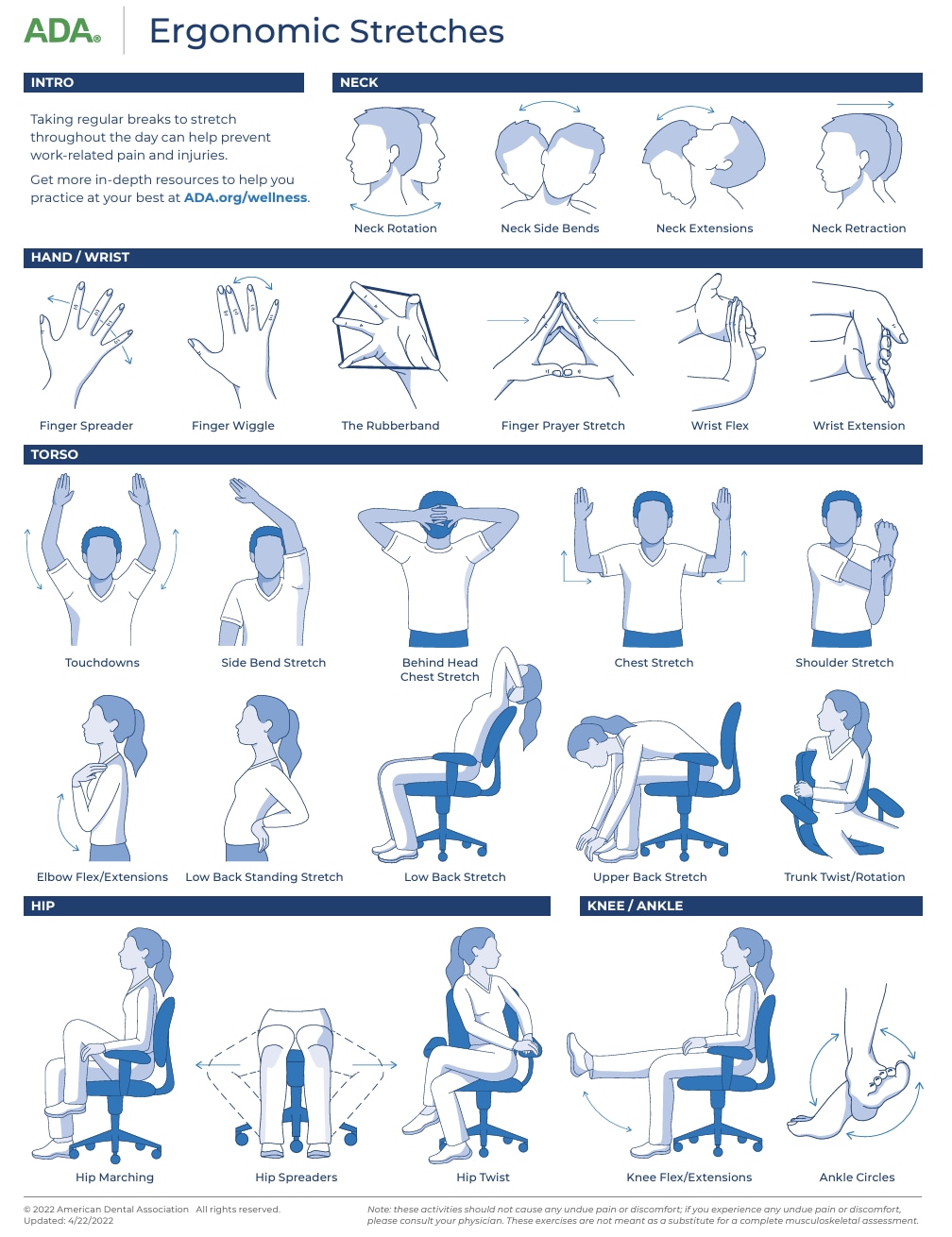
Chairside stretching techniques have been shown to immediately relieve musculoskeletal pain from dentistry and can prevent WMSDs. Studies have shown that any prolonged status postures need contraction of at least 50% of the muscle tissue to prevent tension and trigger points developing. To effectively stretch a tense muscle, it is advised to maintain the stretch slowly for 15-30 seconds which decreases tension. The stretch force should be slow, gentle and pain free. If any pain is felt, the stretch should be stopped for a period before slowly stretching past the point again. It is important to stretch all the muscles used by dental professionals to carry out dental procedures including the hands, wrists, arms, neck, shoulders, back, torso, hips, legs, ankles and feet. A great resource for clinicians to better understand chairside stretches to do between appointments is the American Dental Association Ergonomic Stretches tool (Figure 2).
Muscular Endurance Training
Muscular endurance training that is designed specifically for dental professionals is critical to prevent neck, shoulder and back pain resulting from WMSDs. Dentists are prone to unique muscle imbalances caused by frequent forward head posture and rounded shoulders when treating patients. In addition, maintaining an ideal posture requires good core strength and since the majority of dental procedures are done sitting down, there is not much engagement of the core muscles during long procedures. Strengthening core muscles as well as the middle and lower trapezius muscles for endurance can help maintain ideal posture. The three scapular and three rotator cuff muscles of the shoulders should also be strengthened for endurance so there is less strain and the muscles can tolerate prolonged contraction and load better. Shad Forythe in 2005 suggested a functional training exercise prescription for dental professionals to cover three main categories including torso training (to address spinal cord strength), strength training (both the upper and lower body), and interval training (to address the aerobic endurance of the body).7
Being aware of dental ergonomics and stretches to prevent WMSDs can help ensure longevity in a clinician’s dental career. By intentionally practising in an ideal, ergonomic position as well as setting up the dental surgery for the ideal ergonomics of the auxiliary staff, clinicians can look after their own health, prevent injuries and subsequently provide optimal care to their patients.
Kim E, Jo ED, Han GS. Effects of stretching intervention on musculoskeletal pain in dental professionals. Journal of Occupational Health. 2023;65(1). doi: https://doi.org/10.1002/1348-9585.12413
Kumar DK, Rathan N, Mohan S, Begum M, Prasad B, Prasad ERV. Exercise Prescriptions to Prevent Musculoskeletal Disorders in Dentists. Journal of Clinical and Diagnostic Research : JCDR. 2014;8(7):ZE13-ZE16. doi: https://doi.org/10.7860/JCDR/2014/7549.4620
Ergonomics and posture guidelines for oral health professionals | FDI. www.fdiworlddental.org. https://www.fdiworlddental.org/ergonomics-and-posture-guidelines-oral-health-professionals
Dr. Bethany Valachi PT. Hybrid saddle stools: what’s the scoop? Dental Products Report 2019;53. Accessed April 15, 2024. https://www.dentalproductsreport.com/view/hybrid-saddle-stools-whats-scoop
5 Steps to Improve Your Treatment Room Ergonomics and Avoid Chronic Back Discomfort. Content Library. Published June 14, 2021. Accessed April 15, 2024. https://henryscheinequipmentcatalog.com/content-library/five-steps-to-improve-ergonomics-in-your-treatment-room/
Physical Health & Ergonomics. www.ada.org. Accessed April 15, 2024. https://www.ada.org/en/resources/practice/wellness/physical-health-and-ergonomics
Physical Health & Ergonomics | American Dental Association
Jones AC, Forsythe S. Functional training for dentistry: an exercise prescription for dental health care personnel. Journal of the California Dental Association. 2005;33(2):137-145. doi:10.1080/19424396.2005.12223854
Dr Kaejenn Tchia is a recent graduate working in a corporate private practice in Darwin, Northern Territory. He is the current President of the Australian Dental Association NT Branch Inc. He has also served leadership positions for Bupa Dental Corporation including the Clinical Advisory Panel, Clinical Procurement Committee and currently the Graduate Committee. He is passionate about helping and collaborating with fellow dental colleagues, recently embarking on a new journey to help recent graduates eliminate burnout through a 6-step B.E.L.I.E.F System through his motivational coaching platform, The Limitless Dentist. Kaejenn is a member of the Colgate Advocates for Oral Health Editorial Community and hopes to use this platform to raise awareness of the importance of mental health in dentistry and provide mindset tools, which can help his colleagues unlock their next level of growth and success.
Join us
Get resources, products and helpful information to give your patients a healthier future.
Join us
Get resources, products and helpful information to give your patients a healthier future.











